Week 13 Year 3
Monday, March 29th, 2010This week was my second week at Crosshouse hospital. Crosshouse hospital is classed as the centre of excellence for Cochlear implants in Scotland. After the observation of a few patients attending the department for x-rays to check the position of the implant I then decided to do some research into the subject. I had previously only heard of cochlear implants through my studies of Magnetic Resonance Imaging (MRI) safety, and the contra indications that cochlear implants have with MRI scanning.
A cochlear implant is different from a hearing aid. These devices bypass the damaged portion of the ear and directly stimulate the auditory nerves. Signals generated by the implant are sent by way of the auditory nerve to the brain, which recognises the signals as sound. From my studies of this topic I have found out that hearing through these implants is different from normal hearing and needs to be learnt or relearned. However it does allow people to recognise things like warning signals and understand other sounds and enjoy conversations in person or by telephone.
Both children and adults who are hard of hearing or deaf can be fitted with a cochlear implant. Adults who have lost all or most of their hearing later in life can benefit from these implants, as they learn to associate the signals provided by the implants with sounds they remember. Cochlear implants, along with intensive post-implantation therapy are used as aids to help young children to acquire speech and language.
These implants are used because there is damage or destruction to the hair cells in the cochlear which results in total deafness. However even with this damage the auditory nerve can still be intact.
The cochlear implant works by conveying weak electric stimuli to the vicinity of the auditory nerve. The electric stimulus activates the nerve, which then transmits a signal to the brain. The brain then recognises the signal and the person experiences this as hearing. A cochlear implant has the same function as the hair cells, in that it transforms sound into electric current that stimulates the auditory nerves. This device can help provide a sense of sound to a person who is profoundly deaf or severely hard of hearing.
Hearing is not absolutely normal and research carried out on users who have lost their hearing later in life have stated that the acoustic impressions from the implant differ from normal hearing. Some users describe the sound as, mechanical, or synthetic. This does however change over time and the artificial sound quality is reduced or unnoticed after a few weeks.
Risks from this type of surgery may include facial nerve damage, numbness in the area of the scar, intensification of tinnitus and change in taste sensation and dizziness.
Children who are implanted very young and adults who become deaf later in life, but have already learnt to talk, respond better to the implants than adults with congenital deafness or prelingual deafness. Patients who undergo this operation have to wait 3 to 6 weeks after their operation before beginning training, so any swelling can subside and the initial fitting of the processor can be done. A program consists of 3 phases, firstly adjustment of device. This is adjusted until the patient experiences sounds as being pleasant. Audiological tests are then performed to check whether the adjustments are correct and also to find out what the patient perceives before the training begins. Then last familiarisation with the device and aural training.
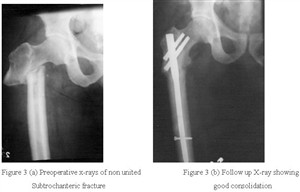
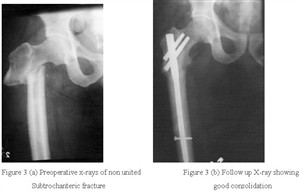
The technique used for imaging patients attending the department for the positioning of a cochlear implant is called modified stenvers which is a project that I was unfamiliar with prior to working at Crosshouse hospital. I found it very interesting to see these projections being undertaken and also understanding the whole patient journey. I was also extremely surprised at how common cochlear implants were and have a better understanding in reference to MRI safety. Attached to this piece of writing are images of cochlear implants and an x-ray image.