This was my second week back at Crosshouse and I had been placed to attend wards and theatres for the week. One particular morning there were two theatre cases which I found to be interesting. The first was a hip arthrogram on a 10 month old girl. The second was for an osteotomy of the hip/femur on an 11 month old female patient. Both had been born with varying degrees of Development Dysplasia of the Hip (DDH).
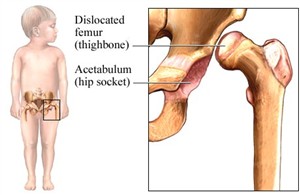
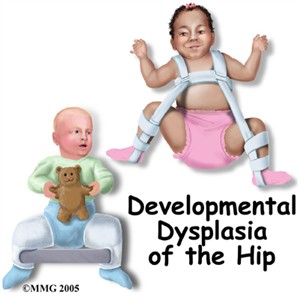
DDH is discovered as part of a routine hip examination check performed on all new born babies. High risk babies are female Caucasian as determined by Pretorius and Solomon (2006). This condition occurs when the formation of the hip joint is dysplastic (abnormal development or growth) or malformed later after birth. The femoral head of the femur and the socket of the acetabulum are made up mostly of cartilage and must be properly orientated for the correct formation. An examination described by Pretorius and Solomon (2006) describes a routine examination on new born babies as the Barlow manoeuvre which dislocates the femoral head rearwards and the Ortolani manoeuvre which reduces the recently dislocated hip usually with a resultant clunk. This examination is carried out for any subluxtion (partially out of alignment) or any instability in the hip joints. Treatments for hip dysplasia depend on the age of the patient. Treatment used for children less than six months of age is a Pavlik harness. The harness holds the hip in an abducted and flexed position. This position allows the best orientation between the femoral head and the acetabulum and allows the hip joint to remodel and develop normally. The harness is then worn full time for six to eight weeks until the hip has stabilised.
The first procedure was an arthrogram of the hip; this was being performed to allow visualisation of the hip joint space and shape. The consultant explained she was hoping to achieve good visualisation of the hip joint to determine any future treatment. An arthrogram is performed by injecting contrast media into the hip joint; this then defines the cartilage surfaces of the joint on an x-ray image. This helps the consultant determine when the hip is reduced and how much instability is present. There is also a possibility if a child reaches about twelve months of age, their hip is difficult to reduce by a closed reduction because the hip socket becomes filled with extraneous tissue and there is secondary contracture of surrounding structures. If this is the case then the patient needs to undergo an open reduction, as in this case the patient required an open reduction.
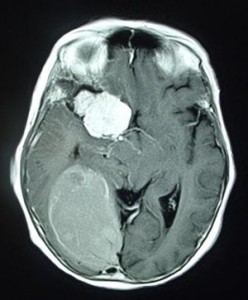
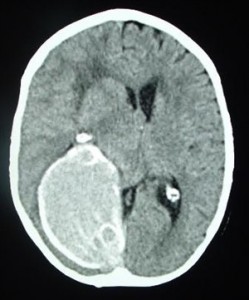
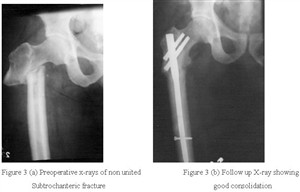
The second patient required an osteotomy. This patient had previously worn a brace to gain shape and stability of her hip; however the hip stabilised with the leg in the wrong position. The surgeon wanted to leave the hip in the joint and cut and realign the femur in the correct position. Attached to this piece of reflection are image from the osteotomy surgery. These images show the new position of the leg and the metal work used to stabilise the position.
Pretorius, S. E. and Solomon, J. A. 2006. Radiology secrets 2nd ed. Philadelphia: Elsevier.
Dislocated femur. 2011. [online image] Available at: http://samsinfo.com/wkl/developmental%20dysplasia%20of%20the%20hip%20ddh%20clicky%20hips.html [Accessed October 20 2010].
Pavlik harness. 2010. Available at; http://www.eorthopod.com/content/developmental-dysplasia-of-the-hip-in-children [Accessed October 20 2010].
Developmental Dysplasia of the hip. 2010. Available at: http://www.pediatric-orthopedics.com/Topics/DDH___Hip_Dysp/ddh___hip_dysp.html [Accessed October 20 2010].
http.web site for hip dysplasia